Table of Contents
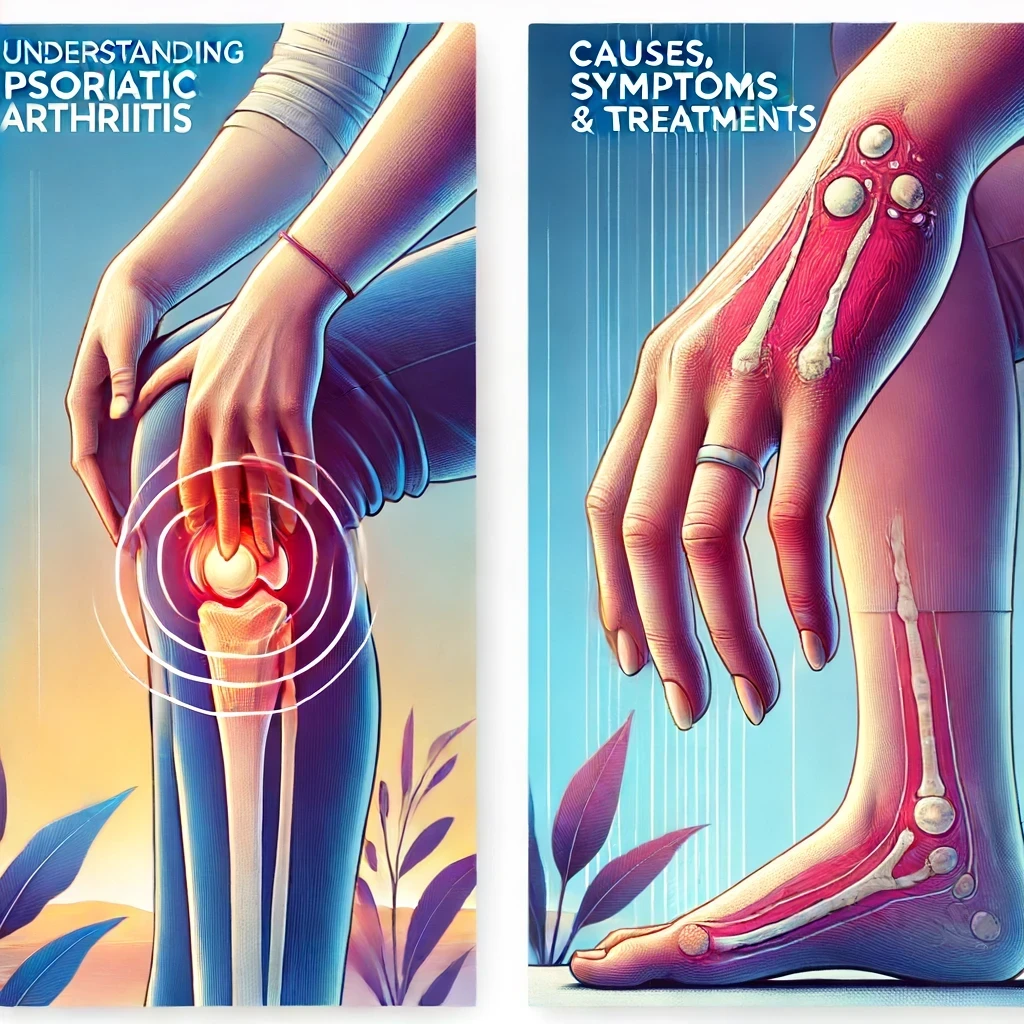
Psoriatic arthritis (PsA) is more than just a combination of psoriasis and arthritis. It’s a unique inflammatory condition that not only affects the joints but also impacts the skin and nails. If you’re grappling with this disease or know someone who is, understanding the nuances of psoriatic arthritis can make managing it a whole lot easier. This comprehensive guide explores the causes, symptoms, treatment options and ways to live better with psoriatic arthritis.
What is Psoriatic Arthritis?
Definition
Psoriatic arthritis is a chronic autoimmune disease characterized by inflammation in the joints and the skin. It belongs to a group of diseases called spondyloarthropathies and is commonly associated with the skin condition psoriasis, which causes red, scaly patches on the skin.
Types of Psoriatic Arthritis
There are several types of psoriatic arthritis, including:
- Symmetric PsA: Affects joints on both sides of the body equally.
- Asymmetric PsA: Affects joints on one side of the body.
- Distal Interphalangeal Predominant PsA: Affects the ends of the fingers and toes.
- Spondylitis: Affects the spine and neck.
- Arthritis Mutilans: A severe form that can cause bone erosion and deformity.
Causes and Risk Factors
Genetic Factors
Genetics play a significant role in psoriatic arthritis. If you have a family member with PsA or psoriasis, your risk of developing the condition is higher. Specific genes associated with the immune system, such as HLA-B27, are linked to PsA.
Environmental Triggers
External factors like infections, stress, or physical trauma can trigger the onset of psoriatic arthritis in individuals who are genetically predisposed.
Immune System Dysfunction
Psoriatic arthritis occurs when the immune system mistakenly attacks healthy cells in the skin and joints, causing inflammation and damage.
Symptoms of Psoriatic Arthritis
Joint Pain and Swelling
Joint pain and swelling are hallmark symptoms of psoriatic arthritis. The joints may feel warm and tender, particularly in the fingers, toes and lower back.
Skin Symptoms
Most individuals with psoriatic arthritis experience skin symptoms associated with psoriasis, such as red, scaly patches. These lesions can be itchy and uncomfortable.
Nail Changes
Nail involvement is common in PsA, leading to pitting, thickening or separation from the nail bed. These changes can be a key indicator of the disease.
Fatigue and Stiffness
Fatigue and morning stiffness are common complaints among those with psoriatic arthritis, often affecting their daily activities and quality of life.
Diagnosing Psoriatic Arthritis
Medical History and Physical Examination
Diagnosis begins with a thorough medical history and physical examination. Doctors look for joint swelling, skin lesions and nail changes that are characteristic of PsA.
Imaging Tests
X-rays, MRI or ultrasound imaging can help assess joint damage and inflammation, providing a clearer picture of the extent of the disease.
Laboratory Tests
Blood tests may be used to rule out other types of arthritis and to detect markers of inflammation, although there is no specific test for psoriatic arthritis.
Differences Between Psoriatic Arthritis and Other Forms of Arthritis
Psoriatic vs. Rheumatoid Arthritis
Both conditions cause joint inflammation, but PsA often affects the spine and the ends of the fingers and toes, while rheumatoid arthritis typically affects the joints symmetrically and spares the spine.
Psoriatic vs. Osteoarthritis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, whereas PsA is an inflammatory condition that also involves the skin and nails.
Treatment Options
Medications
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs help reduce pain and inflammation but do not alter the disease’s progression. They are often used for mild cases.
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs, such as methotrexate, slow down the disease progression and can prevent joint damage.
Biologics and Targeted Synthetic DMARDs
Biologics target specific components of the immune system to reduce inflammation and prevent joint damage. They are often used when traditional DMARDs are ineffective.
Lifestyle Changes
Diet and Exercise
A balanced diet rich in anti-inflammatory foods and regular exercise can help manage symptoms and improve overall health.
Stress Management
Reducing stress through techniques such as yoga, meditation, or therapy can help alleviate symptoms and improve quality of life.
Alternative Therapies
Physical Therapy
Physical therapy can help maintain joint flexibility and muscle strength, reducing pain and improving function.
Acupuncture
Some individuals find relief from pain and stiffness through acupuncture, although scientific evidence is still limited.
Living with Psoriatic Arthritis
Managing Pain and Fatigue
Pain management strategies include medications, physical therapy and alternative treatments. Adequate rest and pacing activities can help manage fatigue.
Tips for Daily Living
Ergonomic tools, joint protection techniques, and energy conservation methods can make daily tasks easier and reduce joint strain.
Emotional Well-being
Managing a chronic condition like PsA can be emotionally challenging. Support groups, counseling and maintaining a positive outlook can significantly help.
Diet and Nutrition for Psoriatic Arthritis
Anti-Inflammatory Foods
Incorporate foods rich in omega-3 fatty acids, antioxidants and fiber to help reduce inflammation. Examples include fish, berries and leafy greens.
Supplements and Nutritional Support
Supplements like omega-3s, vitamin D and turmeric may provide additional support in managing inflammation and joint health.
Exercise and Physical Activity
Benefits of Exercise
Regular exercise can help maintain joint function, reduce stiffness, and improve overall fitness and mood.
Recommended Exercises
Low-impact exercises like swimming, cycling, and yoga are beneficial for individuals with psoriatic arthritis.
Precautions
Always consult with a healthcare provider before starting a new exercise regimen, and listen to your body to avoid overexertion.
The Role of Mental Health in Psoriatic Arthritis
Coping with Chronic Pain
Chronic pain can take a toll on mental health. Developing coping strategies, such as mindfulness and relaxation techniques, can help manage pain more effectively.
Support Groups and Counseling
Connecting with others who have PsA through support groups or seeking counseling can provide emotional support and practical advice.
Latest Research and Developments
New Medications and Treatments
Research is ongoing to develop new biologics and targeted therapies that offer more effective management of PsA with fewer side effects.
Clinical Trials and Studies
Participating in clinical trials can provide access to cutting-edge treatments and contribute to the advancement of psoriatic arthritis care.
Common Misconceptions
Myths about Psoriatic Arthritis
Common myths include that PsA only affects the skin or that it is solely caused by poor lifestyle choices. In reality, it is a complex autoimmune condition with various factors at play.
Fact-Checking Common Beliefs
It’s important to rely on accurate information from reputable sources and healthcare providers when managing PsA.
Future Directions and Hope
Advancements in Treatment
Ongoing research and technological advancements offer hope for more effective and personalized treatments in the future.
Outlook for Patients
With early diagnosis and proper management, many individuals with psoriatic arthritis can lead full and active lives.
Conclusion
Psoriatic arthritis is a multifaceted condition that requires a comprehensive approach to management. From understanding the causes and symptoms to exploring treatment options and lifestyle changes, taking an active role in managing PsA can improve your quality of life. Stay informed, work closely with your healthcare team and embrace a holistic approach to living well with psoriatic arthritis.
FAQs
Can psoriatic arthritis go into remission?
Yes, with effective treatment, some individuals experience periods of remission where symptoms significantly diminish or disappear.
Is psoriatic arthritis hereditary?
Genetics play a role, so if you have family members with PsA or psoriasis, your risk is higher.
How is psoriatic arthritis different from psoriasis?
Psoriasis affects the skin, while psoriatic arthritis affects both the skin and joints, causing inflammation and pain.
Can lifestyle changes really make a difference?
Absolutely! Diet, exercise and stress management can significantly impact symptoms and overall health.
What should I ask my doctor about psoriatic arthritis?
Ask about treatment options, lifestyle modifications, potential side effects of medications and how to manage flare-ups.


One thought on “Understanding Psoriatic Arthritis: Causes, Symptoms and Treatments”